Pembrolizumab/Chemo May Be New Standard in dMMR/pMMR Endometrial Cancer
Investigators report that loss of MMR mechanism is not predictive of response to chemotherapy or pembrolizumab in patients with stage III or IVA, stage IVB, or recurrent endometrial cancer.
“The addition of pembrolizumab to carboplatin and paclitaxel and continued as maintenance was beneficial with respect to a meaningful improvement in progression-free survival [PFS] in both the dMMR and pMMR [populations] independently,” according to lead author Ramez N. Eskander, MD.
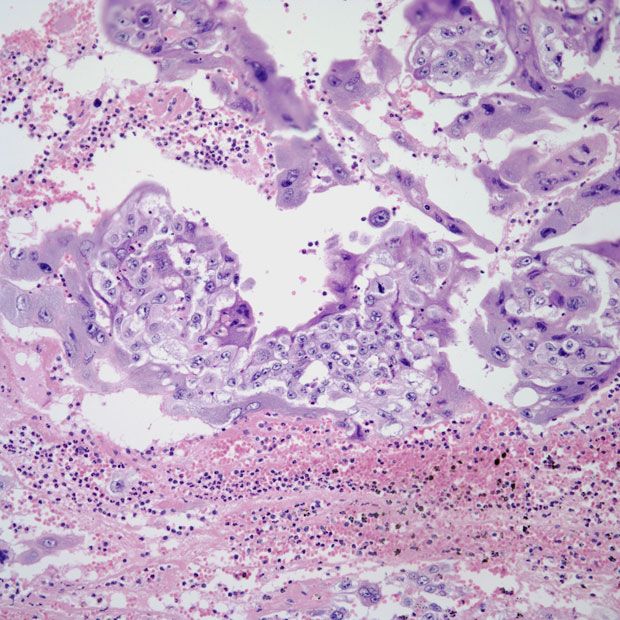
Patients with stage III or IVA, stage IVB, or recurrent endometrial cancer, regardless of mismatch repair deficient (dMMR) or proficient (pMMR) disease status, experienced significant, sustained responses following treatment with pembrolizumab (Keytruda) plus chemotherapy and maintenance pembrolizumab, according to a presentation on findings from the phase 3 NRG GY018 study (NCT03914612) at the 2023 Annual Global Meeting of the International Gynecologic Cancer Society (IGCS).1
In the dMMR population, patients treated with the pembrolizumab combination (n = 92) achieved an overall response rate (ORR) of 82% (95% CI, 72%-89%) compared with 71% (95% CI, 60%-80%) in the placebo arm (n = 92; odds ratio [OR], 1.83; 95% CI, 0.92-3.66). Investigators reported a partial response (PR) rate of 50% vs 55% and a complete response (CR) rate of 32% vs 15% in the pembrolizumab and placebo arms, respectively.
The ORR in the pMMR population was 71% (95% CI, 64%-77%) in the pembrolizumab cohort (n = 212) vs 58% (95% CI, 52%-65%) in the placebo cohort (n = 234; OR, 1.74; 95% CI, 1.18-2.58). Each respective arm achieved a PR rate of 56% vs 50% and a CR rate of 15% vs 8%.
The median duration of response (DOR) in the dMMR population was 28.7 months (95% CI, 20.2-not reached [NR]) in the pembrolizumab cohort compared with 6.2 months (95% CI, 4.3-9.2) in the placebo cohort (HR, 0.218; 95% CI, 0.13-0.37; P <.0001). In the pMMR group, the median DOR was 9.2 months (95% CI, 7.1-14.7) vs 6.2 months (95% CI, 4.8-6.5) in each respective cohort (HR, 0.467; 95% CI, 0.34-0.64; P <.0001).
“The addition of pembrolizumab to carboplatin and paclitaxel and continued as maintenance was beneficial with respect to a meaningful improvement in progression-free survival [PFS] in both the dMMR and pMMR [populations] independently,” lead author Ramez N. Eskander, MD, a gynecologic oncologist and assistant professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, said during the presentation.
“We were subsequently able to confirm an improvement in objective responses and the DOR, and then recognize the relevance of molecular mechanism of MMR loss on outcomes.”
To be included in the study, patients were required to have measurable stage III/IVA or measurable/non-measurable stage IVB or recurrent endometrial cancer. Additional inclusion criteria included having a pathology report with results of institutional MMR immunohistochemistry testing, an ECOG performance status of 0 to 2, and no previous treatment with chemotherapy, with the exception of adjuvant treatment that was completed 12 months or more before the trial.
Patients were stratified based on dMMR vs pMMR status, ECOG performance status, and previous chemotherapy use.
A total of 816 patients—591 of whom had pMMR disease and 225 had dMMR disease—were randomly assigned 1:1 to receive either 200 mg of intravenous pembrolizumab every 3 weeks coupled with 175 mg/m2 of paclitaxel and carboplatin for up to 6 cycles and 400 mg of maintenance pembrolizumab every 6 weeks for an additional 14 cycles, or the same chemotherapy backbone plus placebo and placebo maintenance.
The primary end point was PFS by investigator assessment in both the dMMR/pMMR cohorts, with key secondary end points including safety, ORR, DOR, overall survival (OS) in the pMMR/dMMR cohorts, patient-reported outcomes, and quality of life.
In a previous readout of the NRG GY018 study, investigators reported that the median PFS in the pembrolizumab arm was NR (95% CI, 30.6-NR) compared with 7.6 months (95% CI, 6.4-9.9) in the placebo arm among those with dMMR disease (HR, 0.30; 95% CI, 0.19-0.48; P <.00001).2 In the pMMR population, the median PFS was 13.1 months (95% CI, 10.5-18.8) vs 8.7 months (95% CI, 8.4-10.7), respectively (HR, 0.54; 95% CI, 0.41-0.71; P <.00001).
Investigators also examined PFS by methylation status in those with dMMR endometrial cancer treated with the pembrolizumab combination vs placebo. The median PFS was NR (95% CI, 22.3-NR) vs 7.5 months (95% CI, 6.4-11.3) for those with methylation, and NR (95% CI, 14.2-NR) vs 8.3 months (95% CI, 4.4-NR) with no methylation.
“This was a direct adjudication of promoter hypermethylation. It was not an inferred examination,” Eskander said. “[We] saw two things. In the dMMR population…among patients treated with placebo, the presence or absence of methylation did not appear to be prognostic of outcomes in these patients who received carboplatin and paclitaxel. …Among those who received pembrolizumab, there did not appear to be a significant difference in responses.”
References
- Eskander RN, Sill MW, Beffa L, et al. SEMINAL: Pembrolizumab versus placebo in addition to carboplatin and paclitaxel for measurable stage III or IVA, stage IVB, or recurrent endometrial cancer: the phase 3, NRG GY018 study. 2023 Annual Global Meeting of the International Gynecologic Cancer Society (IGCS). November 5-7, 2023; Seoul, South Korea.
- Eskander RN, Sill MW, Beffa L, et al. Pembrolizumab plus chemotherapy in advanced endometrial cancer. N Engl J Med. 2023;388:2159-2170. doi:10.1056/NEJMoa2302312
Frontline Chemo-Free Regimen Supported in HR+/HER2+ Breast Cancer Therapy
January 1st 2024Combining anastrozole with palbociclib, trastuzumab, and pertuzumab as a frontline therapy for hormone receptor–positive, HER2-positive breast cancer may avoid some of the toxicities associated with chemotherapy, says Amy Tiersten, MD.
Oncology On-The-Go Podcast: ASCO 2023 Recap
June 19th 2023Experts from University of California, Los Angeles Health and Mayo Clinic discuss key data presented at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting in the gynecologic and gastrointestinal cancer spaces and how they may impact patient care.