Metabolic Syndrome Linked to Higher Endometrial Cancer Risk
Women with metabolic syndrome who are age 65 or older have an increased risk of endometrial cancer, according to the results of a new study.
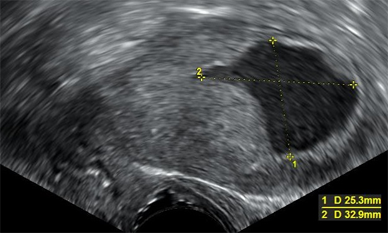
Transvaginal ultrasonography showing uterine fluid accumulation. Biopsy showed endometrioid adenocarcinoma.
Women with metabolic syndrome who are age 65 or older have an increased risk of endometrial cancer, according to the results of a new study published in Cancer Epidemiology, Biomarkers & Prevention. The increased risk was found regardless of whether a woman was also overweight or obese.
Metabolic syndrome is marked by a combination of different medical conditions: low levels of high-density lipoprotein (HDL), the so-called ‘good’ component of cholesterol, and high levels of circulating triglycerides.
Metabolic syndrome, as defined by the US National Cholesterol Education Program Adult Treatment Panel III criteria, was associated with a 39% increased risk of endometrial cancer, or a 21% increased risk after taking into account whether a woman was obese or overweight.
As defined by the International Diabetes Foundation, metabolic syndrome was associated with a 103% increased risk of endometrial cancer, or a 17% increased risk after accounting for whether a woman was overweight or obese.
The case-control study used a SEER and Medicare–linked database of records from 1993 to 2007, analyzing 16,323 women who were diagnosed with endometrial cancer and 100,751 women who lived in the same areas but did not have an endometrial cancer diagnosis.
The researchers also observed that each distinct metabolic syndrome condition that they could evaluate within the database-excessive weight, high blood pressure, high triglycerides, and impaired fasting glucose-was associated with an increased risk for endometrial cancer.
According to senior author Britton Trabert, PhD, a researcher in the division of cancer epidemiology and genetics of the National Cancer Institute in Bethesda, Maryland, about one-fourth of people who do not have diabetes have metabolic syndrome.
While the study did not directly seek to understand how prevention of metabolic syndrome affects the incidence of endometrial cancer, the study showed that exercise and weight loss could be effective in preventing metabolic syndrome.
Prior studies have shown that obesity is a major risk factor for endometrial cancer. While studies have also shown a link between metabolic syndrome and a higher endometrial cancer risk, whether this link was due to obesity-which is also linked to metabolic syndrome-was unclear. The current results add to the evidence that metabolic syndrome contributes to the risk of endometrial cancer.
The current study, according to the authors, is the first to report on the link between metabolic syndrome and different endometrial cancer subtypes. The study shows that metabolic syndrome results in a stronger increased risk of mucinous endometrial tumors compared with low-grade endometrioid tumors.
“Strategies to reduce the prevalence of metabolic syndrome factors might have a favorable effect on the incidence of endometrial cancer,” conclude the study authors.