68 Magnetic Tracer Increases Surgical Productivity and Reduces Time to Surgery When Compared With Standard Lymph Node Mapping Modalities
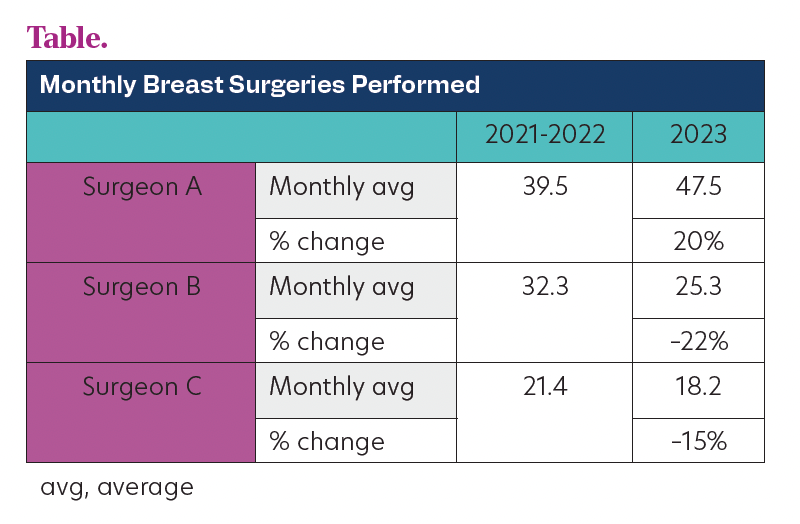
Table. Magnetic Tracer Increases Surgical Productivity and Reduces Time to Surgery When Compared With Standard Lymph Node Mapping Modalities
Background
Delayed cancer surgery is a core challenge faced by large-volume hospitals. This is influenced by long workups, operating room (OR) access, scheduling across multiple service lines, and continuing institutional cost pressures. The Commission on Cancer recommends that breast surgery be performed within 60 days of diagnosis. Standard tracers contribute to delays due to scarcity of products and appointments and increase in efficiency and cost due to multiple patient visits. A nonradioactive magnetic tracer (Magtrace) can replace a standard tracer, resulting in reduced cost and increased OR utilization. The aim of this study was to investigate the impact of the magnetic tracer (MT) on hospital workflows in a high-volume nonacademic medical center.
Methods
A retrospective analysis of 3 surgeons (A, B, C) over 3 years (March to August of 2021, 2022, and 2023) performing breast surgery. Surgeon A adopted the MT in March 2023 while B and C continued with Tc99 and blue dye. Outcomes collected included the number of surgeries performed, the number of days between referral and surgery, and the supply costs of the tracers.
Results
A total of 1665 patient records were analyzed (Table). Post MT adoption, surgeon A saw an increase in monthly breast surgical volume by 8 additional surgeries (47.5 in 2023 vs 39.5 in 2021-22, P = .0882). Surgeons B and C observed a decrease in volumes (surgeon B, 25.3 patients vs 32.23, P = .0133; surgeon C, 18.2 vs 21.4, P = .2468). Surgeon A experienced a reduction in the average time from referral to surgery by 11 days (from 80 to 69 days). The cost analysis revealed that MT was $656.65 per patient whereas the average Tc99 cost was $854.66 and isosulfan blue (BD) was $979.73. Per-patient cost savings were $198.01 when compared with Tc99 alone and $1177.74 when compared with Tc99 and BD.
Conclusions
Although there are many factors contributing to OR access and surgeon volume, the use of MT in a high-volume, nonacademic United States center may increase surgical volumes and reduce the time from referral to surgery. This approach not only improves hospital efficiency but also offers potential cost savings and scheduling benefits. These finding suggest that the MT may contribute to broader efficiencies in cancer care and may facilitate COC compliance. Further data collection is underway to monitor trends over time with wider adoption of the MT platform across surgeons.
