FLT-PET Fails to Distinguish True Glioblastoma Progression
Positron emission tomography using [18]F-fluorothymidine as a tracer failed to distinguish true progression of glioblastoma from pseudoprogression in a small single-center study presented at the 2014 ASCO Annual Meeting.
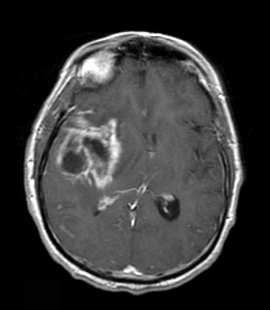
Pseudoprogression—MRI of a patient with a glioblastoma at 6 weeks post-chemoradiation demonstrating an initial increase in enhancement mimicking progressive disease.
CHICAGO-Positron emission tomography (PET) using 18F-fluorothymidine (FLT) as a tracer failed to distinguish true progression of glioblastoma from pseudoprogression in a small single-center study presented Saturday at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting.
Glioblastoma is typically treated with surgery plus 6 weeks of radiotherapy plus temozolomide, followed by 4 weeks of rest, followed by 6 courses of adjuvant temozolomide.
“One of the problems that arises with this treatment is pseudoprogression, defined as progressive contrast enhancing lesions on MRI after chemoradiotherapy followed by stabilization or reduction in these lesions without change of therapies after 3 cycles of adjuvant temozolomide,” said study presenter Martha W. den Hollander, MD, of University Medical Center Groningen, the Netherlands. “This is normally seen in up to 64% of patients with progressive disease on MRI after chemoradiotherapy.”
In this study, den Hollander and colleagues wanted to examine the use of FLT-PET in distinguishing between true progression and pseudoprogression in patients with primary glioblastoma. FLT is a tracer that is taken up by proliferating tumors cells.
The study included 30 patients, 28 with glioblastoma and 2 with gliosarcoma; 24 patients underwent assessment for pseudoprogression. The researchers compared changes in maximum standardized uptake value (SUVmax) and tumor to normal brain tissue ratios between patients with pseudoprogression and true progression. True progression was defined as progressive disease after chemoradiotherapy and further progression after three courses of temozolomide.
Of the 24 patients analyzed for pseudoprogression, 10 had stable disease or complete response after chemoradiotherapy and 14 had progressive disease. Of the 14 patients found to have progressive disease, 7 had pseudoprogression and 7 had true progression.
The researchers found no difference in SUVmax and tumor to normal brain tissue ratios on FLT-PET between patients with true progression compared with pseudoprogression. However, the researchers did find that baseline FLT uptake was associated with overall survival. The median uptake of all 30 patients was 1.59 SUVmax.
“Patients with an uptake lower than 1.59 had a higher overall survival than patients with an SUVmax higher than 1.59,” den Hollander said.
The median overall survival was 9.5 months for patients with a higher SUVmax compared with 20 months for patients with an SUVmax less than 1.59 (P = .01).
In a discussion of the results of this study, Elizabeth Robins Gerstner, MD, of Massachusetts General Hospital, commented on the increasing interest in looking at PET imaging in brain cancers. Gerstner acknowledged that PET does provide information about metabolism that is unavailable with MRI; however, she also pointed out that PET has several limitations as well, including being nonspecific, providing only a static picture of the tumor’s metabolism, and a lack of standardization of acquisition protocols.
“PET does provide complementary information to MRI and may be useful in certain scenarios where MRI does not show us what is going on,” Gerstner said. “However, to optimize the usefulness of PET we do need to be thoughtful about how the tracer is metabolized and our parameters for selection for what we are measuring and associating with our outcome variable.”
Oncology On-The-Go Podcast: ASCO 2023 Recap
June 19th 2023Experts from University of California, Los Angeles Health and Mayo Clinic discuss key data presented at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting in the gynecologic and gastrointestinal cancer spaces and how they may impact patient care.